Understanding the Blank Soap Note Template
A blank soap note template serves as a standardized document used by healthcare professionals to record patient encounters. It provides a structured framework for documenting essential patient information, including the patient’s history, physical examination findings, diagnosis, and treatment plan. A well-designed template not only ensures consistency in documentation but also enhances communication and improves patient care.
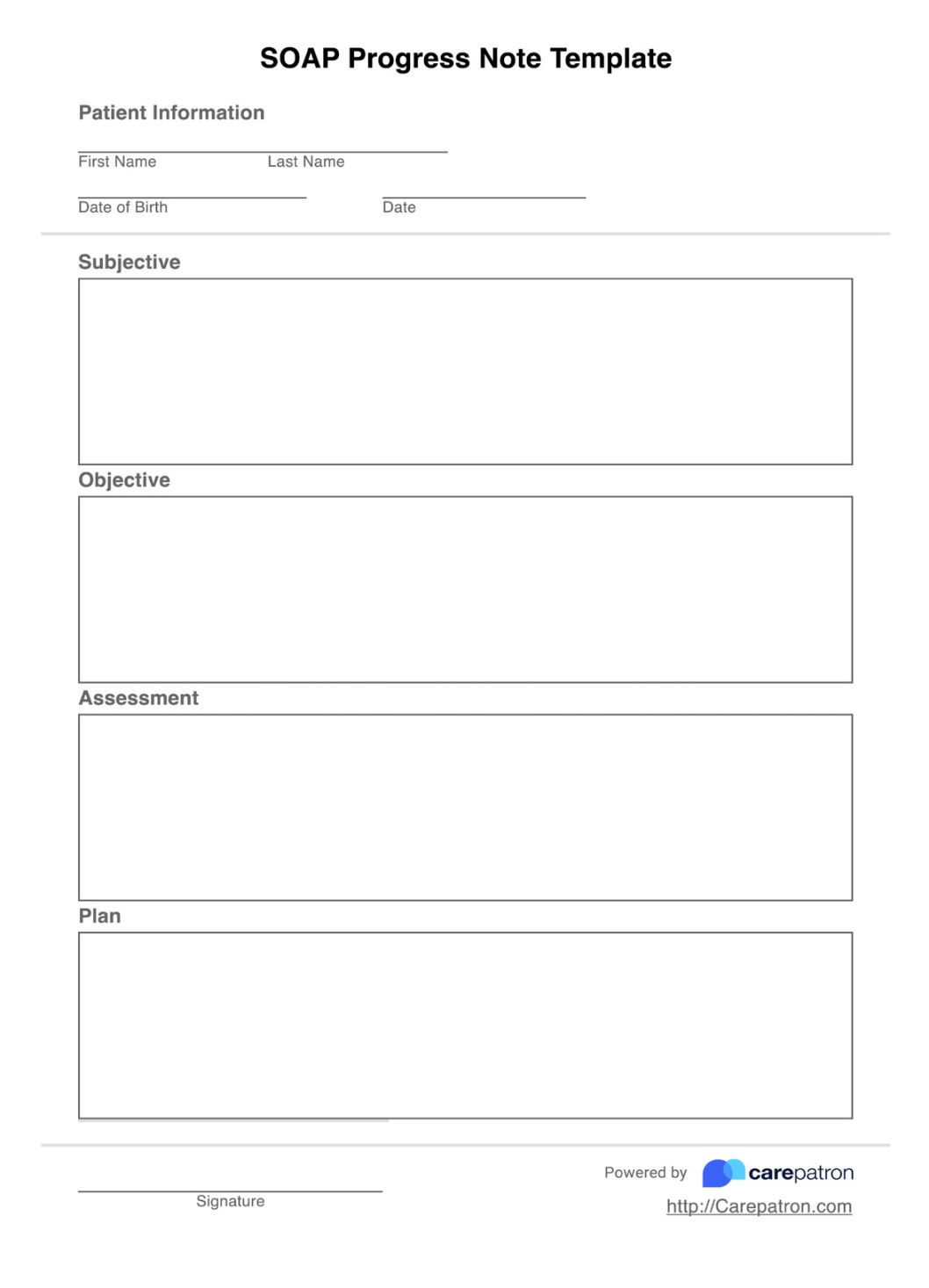
Key Elements of a Blank Soap Note Template
1. Patient Information: This section should include the patient’s name, date of birth, medical record number, and date of the encounter.
2. Subjective Information: This section captures the patient’s self-Reported symptoms, concerns, and any relevant medical history.
3. Objective Information: This section details the healthcare provider’s observations and findings, such as vital signs, physical examination results, and laboratory or diagnostic test results.
4. Assessment: This section summarizes the healthcare provider’s diagnosis or working diagnosis based on the subjective and objective information.
5. Plan: This section outlines the treatment plan, including medications, procedures, referrals, and follow-up appointments.
Design Elements for a Professional Blank Soap Note Template
1. Layout and Formatting:
2. Font Selection:
3. Color Scheme:
4. Branding and Customization:
5. Accessibility:
Example of a Professional Blank Soap Note Template
Patient Information:
Name:
Subjective:
Chief Complaint:
Objective:
Vital Signs:
Assessment:
Plan:
Medications:
Conclusion
A well-designed blank soap note template is essential for efficient documentation and effective communication in healthcare settings. By incorporating the key elements and design principles outlined in this guide, healthcare professionals can create templates that are both professional and functional, ultimately improving patient care.